The Medicalization of Psychiatry
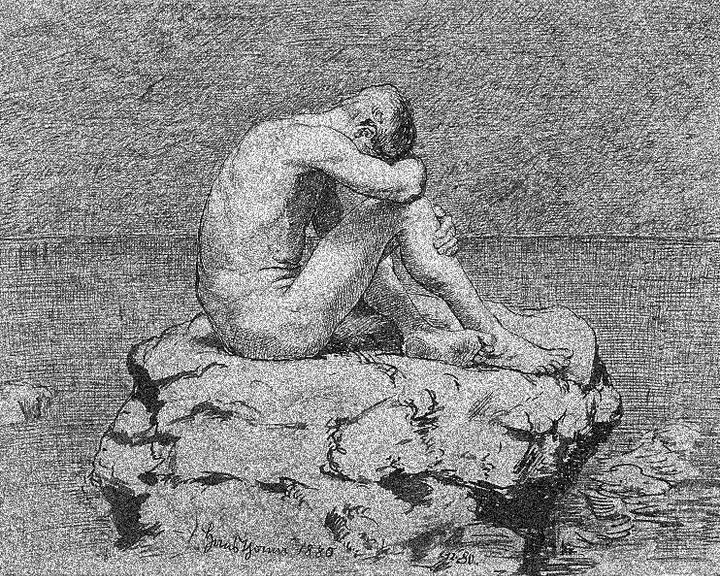
Patients are reduced to containers for diagnoses and psychiatrists to abstract functionaries.
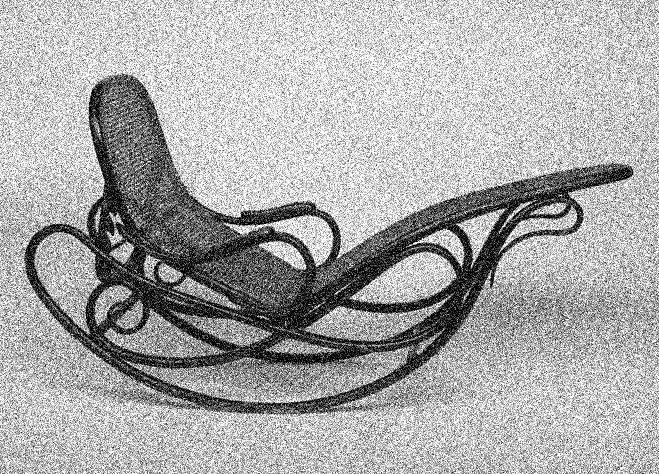
Cruelty that originates in good intentions is particularly dangerous and difficult to recognize. The conceptual medicalization of psychiatry is an instance of such cruelty. Medical practices like lobotomy, incarceration and pharmacological assault are obviously horrific, but similar patterns underpin the shift in the way psychiatrists came to think about their patients in the mid-twentieth century. Psychiatrists moved their primary focus from personal attention to patients to eradicating supposed illnesses or disorders. The primary means of this of this subtle but profound change were the introduction of a new diagnostic system and “evidence-based” methodology into psychiatry.
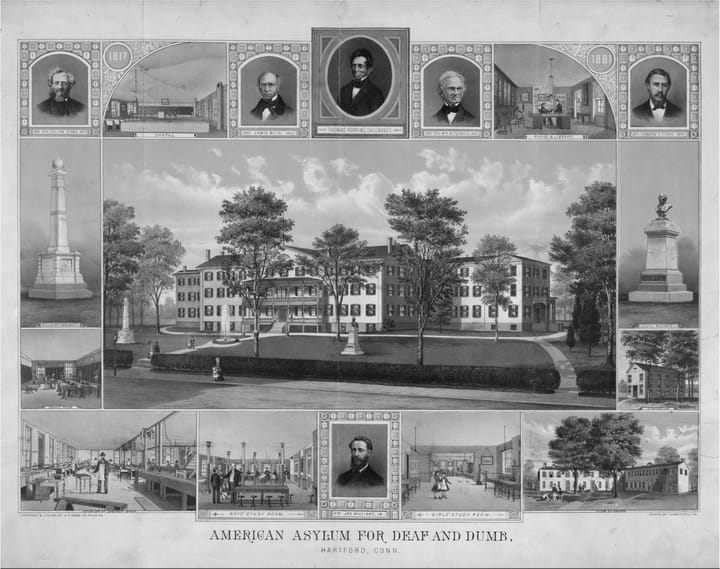
Starting in the 1960’s American psychiatrists began a movement to establish psychiatry as a “branch of medicine,” not only in the sense that psychiatrists should have preeminence in treating people whose psychology or behavior was non-normative, but more importantly that they should think in the same manner as other physicians. Following the incredible success of antibiotics in treating specific diseases after WWII, this meant a focus on treating well-specified disorders whose diagnoses carried a clear picture of what was wrong, what would happen if the condition ran its course, and the likely effects of various interventions. The key to this approach lay in the categorization of disorders that integrated cause, outcome and therapeutics. In this manner, psychiatrists sought to define disorders in a way consistent with Socrates’s call to “carve nature at its joints.”
The new psychiatrists’ approach seemed consistent with the previous decade’s advances in the pharmacological treatment of psychiatric disorders and the rapidly increasing knowledge of brain function, although neither of these developments bore any logical connection to the proposed diagnoses. (A single exception was the chemical Lithium, which was accidentally discovered to have a specific effect on bipolar disorder.) Labeling themselves neo-Kraeplineans after Freud’s contemporary Emil Kraeplin, they thought of themselves as re-grounding psychiatry in the categorization of clear and visible features rather than the elaborate theories of psychoanalysis.
The major product of this effort was the DSM-III and its successors, a supposedly atheoretical classificatory manual of psychiatric disorders based in directly observable signs and symptoms. The DSM avoided psychoanalytic formulations as “unscientific,” but also on account of the personal affronts inflicted by an arrogant psychoanalytic community. Although it quickly became apparent that the DSM was a poor attempt to accomplish even its limited classificatory goals, it nonetheless came to dominate American psychiatry.
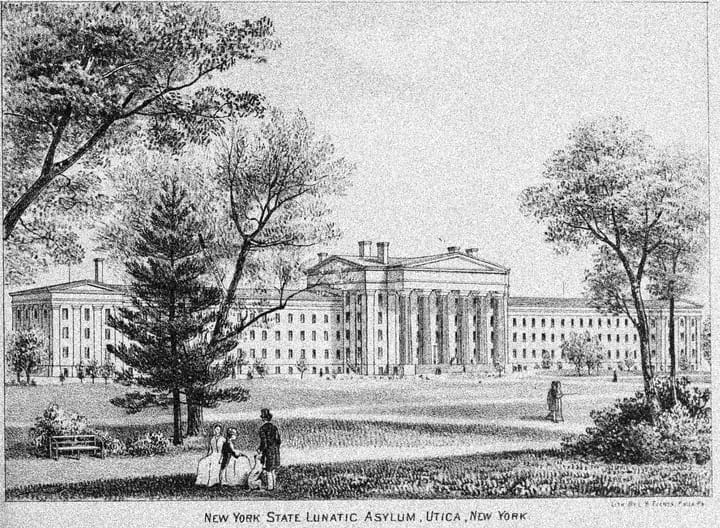
Prior to the introduction of the DSM-III, American psychiatrists were expected to produce “case formulations,” or multiple-page narratives of a patient’s life. The DSM shifted attention away from the patient’s life to the problem of illness classification. This shift was part of a broader trend in medicine, which turned patients into mere bodies to be worked upon. Cancer is the most dramatic example: the “war against cancer” was fought on a battleground that happened to be a person’s body, often with little attention to the devastation that resulted from that war. Psychiatry followed suit.
The long-standing tendency to mistreat individuals in psychological distress had been momentarily disrupted by the psychoanalytic movement, which insisted that the apparently senseless symptoms of mental disturbance were full of meaning and connected to shared human motivations. For approximately a quarter of a century following the WWII, the view that the “mentally ill” suffered from repressed thoughts and experiences dominated academic psychiatry and much of psychiatric practice. Psychoanalyst Harry Stack Sullivan’s claim that “schizophrenics are more human than otherwise” epitomized the view that the difficulties of psychiatric patients were best understood as variations of ordinary human experience, and that psychiatric patients should be treated accordingly. Whatever its failings, psychoanalysis recognized patients as human, and it was this basic insight from which the new psychiatry turned away.
The surgical joke, “the operation was a success, but the patient died,” is unfortunately reflective of much current psychiatric thinking, in which the overall well-being of patients is less important than the disappearance of their signs and symptoms. Although this cruel attitude doubtless has multiple sources, the medicalization of psychiatry is the driving cause. It serves as a rationalization for cruelty in the same way that the “war on crime” serves as a rationalization for the outrageous incarceration of an enormous portion of our population.
People come to psychiatrists because they are in distress or they are distressing someone else. They hope the psychiatrist will show them a route out of that distress and that this initial encounter will provide them with sufficient hope to follow the psychiatrist’s advice. In other words, they hope to come away from the meeting with a sense of alliance with a trusted other who will help them with their suffering. A minimum prerequisite for the development of such trust is that the psychiatrist is interested in the patient’s well-being, willing to learn what the difficulty is, and competent to help.
In the psychoanalytic tradition and in the older psychiatric tradition, a diagnostic evaluation consists of “getting to know the patient”: discovering their world and attempting to place their difficulties within the context of their entire lives. It focuses on questions like who and what are important to the patient, how symptoms affect the patient’s life, what the patient understands and feels about their symptoms, and what the patient hopes for from the psychiatrist. The psychiatrist’s search for answers to these questions is a reflection of their commitment to the patient’s well-being.
The medical psychiatrist, by contrast, must answer the question of which diagnostic category suits the patient and, by extension, which evidence-based treatment should be prescribed. The patient interview will center on a long series of questions designed to discover the presence or absence of categorizing symptoms and the appropriateness of various interventions. Psychiatrists today are encouraged to follow an outline that systematically inquires into a range of symptoms intended to differentiate a number of diseases. It’s alienating for the therapist to check a box rather than offer a human response.
Furthermore, much of the current practice of psychiatry consists in “med checks”: 10 to 15 minute meetings with a psychiatrist to see whether prescribed medications are working and whether side effects are present. It is impossible in this time to do more than ask these highly specific questions, although at some facilities patients are informed that if there is “something to talk about” (as if there ever isn’t), arrangements can be made to see a therapist. Med checks began in the 1960’s as means of managing the large populations that were discharged from chronic psychiatric hospitals. This mass exodus followed from the discovery that new antipsychotic drugs could sufficiently control behavior so that most patients did not require hospitalization. For some, who found talking about themselves unrewarding or painful, med checks provided a way to receive medication in a less distressing way. But with medicalization, med checks became standard care, satisfying the requirement of integrating diagnostic focus with evidence-based care.
Med-check psychiatry, as demanding as it is dull, is now the norm thanks to the enormous economic incentives for psychiatrists. Placing the complexities of real life outside the attention of psychiatrists, it has simultaneously dehumanized patients and left them without help in central areas of their lives. It has also dehumanized psychiatrists themselves, making them into robots who are required to blind themselves to the humanity of the people they encounter.
There are obviously financial incentives for medicalized thinking, but a not-so-latent wish also undergirds its blindness: the wish to differentiate the supposedly healthy psychiatrist from the supposedly ill patient. The medical model thus gives psychiatrists reason to think that they are qualitatively different from the people they treat. Patients are reduced to containers for diagnoses and psychiatrists are reduced to abstract functionaries by a practice that categorizes illness rather than treats people.
■
Robert M. Galatzer-Levy, M.D. is Clinical Professor (P.T.) of Psychiatry and Behavioral Neuroscience at the University of Chicago Pritzker School of Medicine, and on the faculty at the Institute for Psychoanalysis in Chicago. His interests include clinical psychoanalysis, nonlinear dynamical systems theory, and forensic psychiatry. His most recent book is Nonlinear Psychoanalysis: Notes form Forty Years of Chaos and Complexity Theory.